Tell me your country, how you live, and I’ll tell you your risk of type 2 diabetes
Although it is fairly well known around us that the risk of type 2 diabetes is higher at lower income and cultural levels, in developing countries it is just the opposite
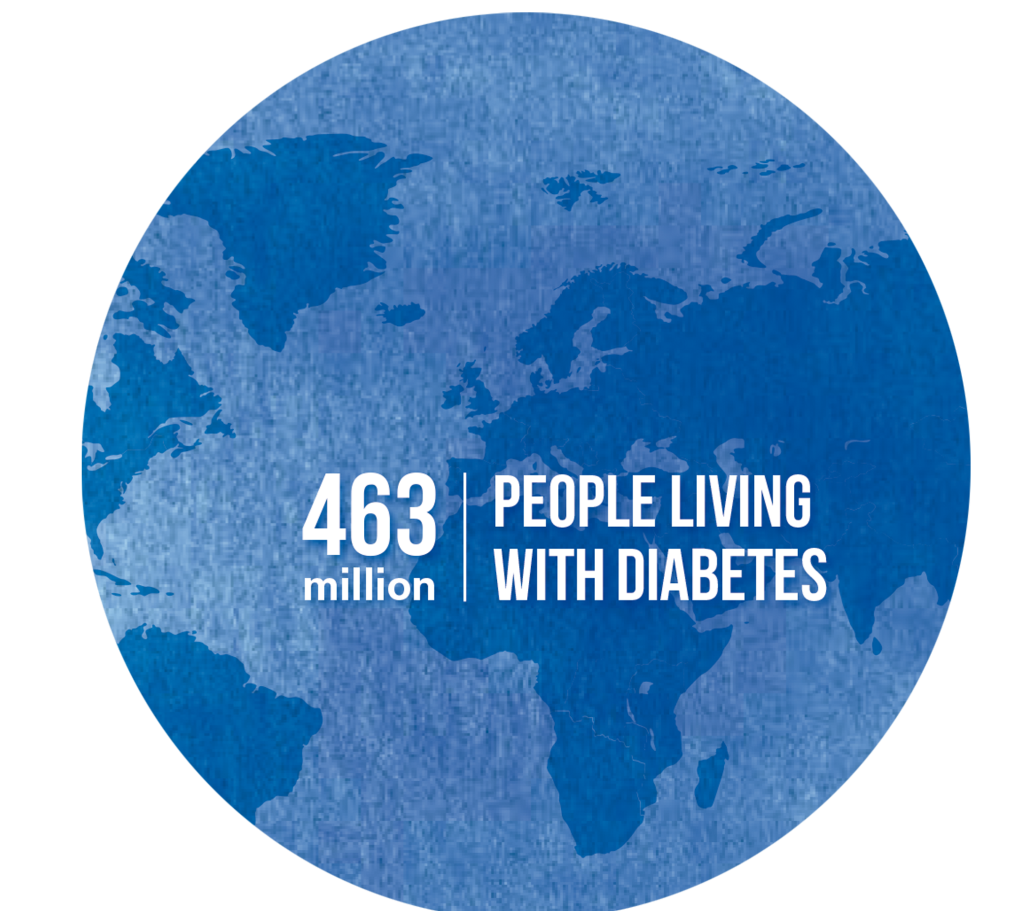
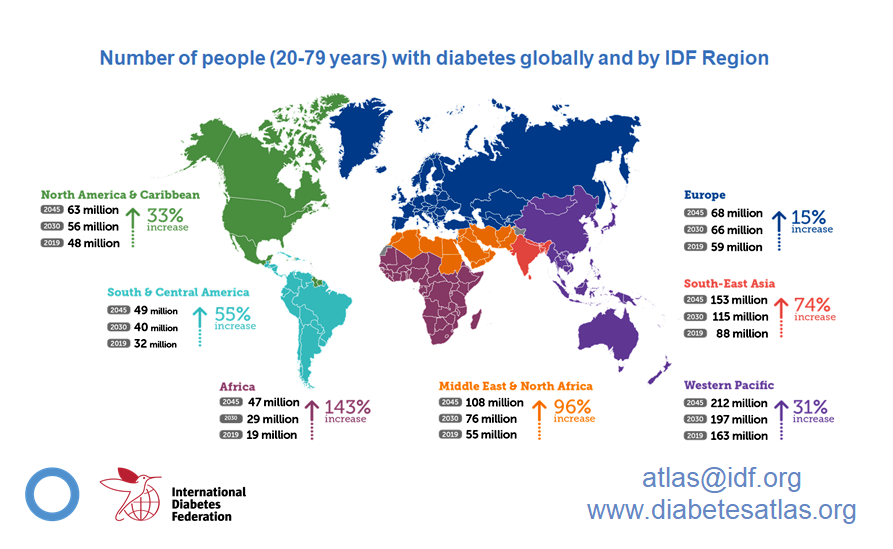
Type 2 diabetes is considered the fastest growing chronic disease in the world. The most 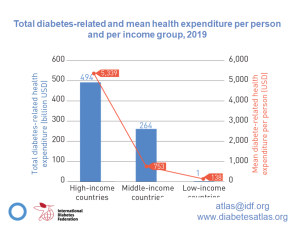 up-to-date data from the World Diabetes Atlas (published regularly by the International Diabetes Federation, IDF) states that if by 2019 we have an estimated 463 million people with diabetes worldwide, by 2045 this figure is projected to be around 700 million. Thus, on average and within the global picture, it is estimated that one death from diabetes or its complications occurs every 8 seconds. The IDF estimates that the annual direct cost of diabetes worldwide is USD760 billion. By 2030 and 2045, these direct costs are projected to reach USD825 billion and USD845 billion, respectively. To this should be added the indirect cost (from premature death, disability and other diabetes-related complications), which is estimated to increase the direct cost by 35%.
up-to-date data from the World Diabetes Atlas (published regularly by the International Diabetes Federation, IDF) states that if by 2019 we have an estimated 463 million people with diabetes worldwide, by 2045 this figure is projected to be around 700 million. Thus, on average and within the global picture, it is estimated that one death from diabetes or its complications occurs every 8 seconds. The IDF estimates that the annual direct cost of diabetes worldwide is USD760 billion. By 2030 and 2045, these direct costs are projected to reach USD825 billion and USD845 billion, respectively. To this should be added the indirect cost (from premature death, disability and other diabetes-related complications), which is estimated to increase the direct cost by 35%.
Will it be my turn, will it be your turn?
The risk determinants of type 2 diabetes have typically focused on certain metabolic and physiological variables such as weight, waist circumference, blood pressure, etc. But if we take a step back, we can see that these target values can be related to lifestyles and genetics. It is not by chance that the IDF itself claimed in its 2015 report that proper lifestyle habits could prevent 70% of type 2 diabetes cases.
But in many cases, it is useful to look at the extent to which the socio-economic status of a group can lead to predicting their risk of type 2 diabetes. The fact is that it is quite well established that, in general, those groups with a worse socioeconomic position have, at the same time, worse lifestyles: they smoke more, drink more, their dietary quality is worse and, again in general, they are more sedentary.
The 2017 paper entitled “Socio-economic status is associated with the prevalence of diabetes in the global picture” is as eloquent as its title. But it found that the relationship was inversely related to the level of development of the country concerned. That is, the prevalence of diabetes was directly correlated with the so-called ‘Human Development Index’ (or HDI*). To summarize more graphically, in poor countries diabetes affects a greater proportion of higher income groups, and in rich countries the opposite is true for lower income groups.
Diabetes repeats the story of obesity
A personal comment on these findings: Data highlighted, again, in this recent study by contrasting that, in China, having a higher income and a non-manual occupation was associated with a higher prevalence of type 2 diabetes, which was also predicted by the body mass index.
Not long ago, obesity was a feature associated with countries that were developing. But, unlike today, that obesity was more visible within the framework of a certain socio-economic status. It was a time when “corpulent” people (at that time they were not called “obese”) were represented in a caricatural way by that gentleman who in his maturity wore a hat, a Levite, a Havana cigar and a lady to match (she with long pearl necklaces).
However, nowadays, obesity (no longer called “corpulence”) is, in our environment, much more prevalent, more common, in those socially and economically depressed groups. Obesity has changed sides, as has diabetes.
This drift is to some extent associated with the concept of “nutritional transition”. A process in which a society moves from an environment characterized by food scarcity to another, opposite, environment characterized by overabundance. It goes without saying that in that environment of food shortage many of the health complications are related to nutritional deficiencies, famine, etc.; and that the second scenario (ours and the current one) is “embellished” with the diseases typical of superabundance, which begin, for instance, with diabetes.
process in which a society moves from an environment characterized by food scarcity to another, opposite, environment characterized by overabundance. It goes without saying that in that environment of food shortage many of the health complications are related to nutritional deficiencies, famine, etc.; and that the second scenario (ours and the current one) is “embellished” with the diseases typical of superabundance, which begin, for instance, with diabetes.
Thus, the relationships between concepts such as “nutritional transition”, “obesity transition” and finally “diabetes transition” seem more than evident. Diabetes is simply running on the same tracks that obesity. After all, weight, BMI, waist circumference, etc. are physiological variables that are closely related to type 2 diabetes. This way of “evolving” was highlighted a few months ago in The Lancet’s publication “The Obesity Transition: the stages of a global epidemic” when three stages were observed in relation to the transition of this obesity and its socio-economic characteristics:
- Stage 1: higher prevalence among higher socioeconomic groups.
- Stage 2: reduction of differences between groups with different socioeconomic status
- Stage 3: socio-economic differences from stage 1 are reversed due to a greater acceleration of obesity among subpopulations that previously had a lower BMI
In summary
From a theoretical point of view, it may be more or less curious to contrast how the risk of suffering from type 2 diabetes correlates with the socio-economic status of each individual, and that its meaning, whether it is greater or lesser, depends in turn on the level of development of the country we are considering. In our environment, the most economically disadvantaged groups have a greater risk of suffering from it. However, these data are of no value when the individual becomes aware of the importance of his or her life habits. Therefore, beyond the role that states and their respective health administrations have to establish public health policies aimed at reducing the differences between groups, the involvement of families is crucial in order to adopt better life habits.
*Human Development Index: This is a statistical tool used to measure the extent to which a country has social and economic dimensions that end up impacting on health, education and living standards. You have more information about it, as well as about obtaining it, in this link.
Latest posts by Juan Revenga Frauca (see all)
- Obesity recognized as a chronic disease - 13 October, 2021
- Who said you have to eat everything? - 7 October, 2021
- Diabetes and Alzheimer - 29 January, 2021